Supplemental Content
AKI Staging
CKD Staging and Risk Assessment
Renal dysfunction, including acute kidney injury (AKI, a subset of acute kidney disease [AKD]) and chronic kidney disease (CKD), can stem from a wide variety of etiologies, such as chronic disease, trauma, exposure to nephrotoxic drugs, or major surgery. Because of the kidneys’ vital and diverse functions (ie, excretory, endocrine, and metabolic) within the body, renal damage or impairment can lead to potentially severe complications and sequelae.
When CKD or AKI is suspected based on patient history, risk, exposure, and/or susceptibility, markers such as the following can be used in diagnosis and staging , , , :
- Serum creatinine, measured
- Urine output, measured
- Urine albumin-to-creatinine ratio (uACR), measured
- Glomerular filtration rate (GFR), either measured or estimated
- Serum cystatin C, measured
In addition, clinical assessment and testing should be performed to determine etiology, which may impact treatment decisions.
Quick Answers for Clinicians
In general, the diagnostic approach for suspected kidney dysfunction relies on whether acute kidney injury (AKI) is suspected. When AKI is suspected, urinary output and serum creatinine measurements are recommended as proxies for glomerular filtration rate (GFR); estimated GFR (eGFR) is less accurate when creatinine concentrations are changing rapidly. Reductions in urinary output can be detected sooner than increases in serum creatinine, and diagnosis of AKI requires only one of the two criteria (ie, creatinine increase or urinary output decrease) to be met.
By contrast, recommended testing in the setting of longer-term kidney disease (without acute injury) includes eGFR and urine albumin-to-creatinine ratio (uACR), both of which play an important role in estimating the risk of complications and negative outcomes.
In 2021, a joint task force of the National Kidney Foundation and American Society of Nephrology released new recommendations to discontinue use of the 2009 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equations for estimating glomerular filtration rate from creatinine (eGFRcr) and creatinine with cystatin C (eGFRcr-cys), both of which include a race coefficient. The task force further recommended immediately implementing the 2021 CKD-EPI equations, which omit race as a coefficient, in adult patients:
Use of the 2012 CKD-EPI equation derived from cystatin C only is unaffected by these new recommendations because it does not include a race coefficient.
For many individuals, these updated equations will have little to no impact on clinical management; however, eGFR calculations may be more meaningfully altered in Black individuals, younger adults, and patients with low creatinine concentrations.
Creatinine is generally a reliable endogenous marker of renal function, as it is produced in relatively consistent quantities each day in a given individual. However, there are many clinical scenarios in which creatinine may be less dependable. For example, creatinine measurements will be less reliable in patients with low muscle mass or conditions that impact creatinine production or elimination. Certain drugs (eg, trimethoprim, fenofibrate, cimetidine, etc.) are also known to affect creatinine levels. Finally, spectral and chemical interferences (eg, ketones, glucose, beta-hydroxybutyrate, cephalosporins, bilirubin, lidocaine, etc.) can affect alkaline picrate and enzymatic testing. ,
When any such issue is anticipated, guidelines recommend additional testing to confirm creatinine-based results. Use of cystatin C or another renal clearance marker is suitable for confirmation. However, similar care should be taken to identify any circumstances in which cystatin C measurements may be impacted (eg, obesity, history of transplant, cigarette use, malnourishment, etc).
Yes. Although recommendations for pediatric and adult populations overlap in terms of testing and diagnostic criteria, variation remains in areas such as diagnostic thresholds, staging, and glomerular filtration rate (GFR) estimation. Notably, the recommended 2021 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equations for estimating GFR are currently validated for use in adults only. For specific information on pediatric testing, refer to the Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines on acute kidney injury (AKI) and chronic kidney disease (CKD).
Acute Kidney Injury
AKI is an abrupt and time-limited subset of AKD that can result from a wide range of situations, such as trauma, toxic exposure, and renal obstruction. It can be defined as renal impairment lasting for up to 7 days.
Laboratory Testing
When AKI is suspected, serum creatinine and urinary output should be measured to assess renal impairment. In AKI, urinary output decreases before creatinine concentrations increase; initial diagnosis of AKI can be based on either urinary output or creatinine concentrations, whichever marker is available first. Patients who meet any creatinine or urinary output staging criteria for a period of 1 to 7 days can be considered to have AKI.
The frequency and duration of AKI monitoring should be determined on an individual basis according to patient risk (including any exposures or susceptibilities) and progression. Serum creatinine should be tested a minimum of two times during a period of 48 hours, or in high-risk patients, at least daily. Urine output monitoring should be considered in patients who are critically ill.
AKI Diagnosis and Staging
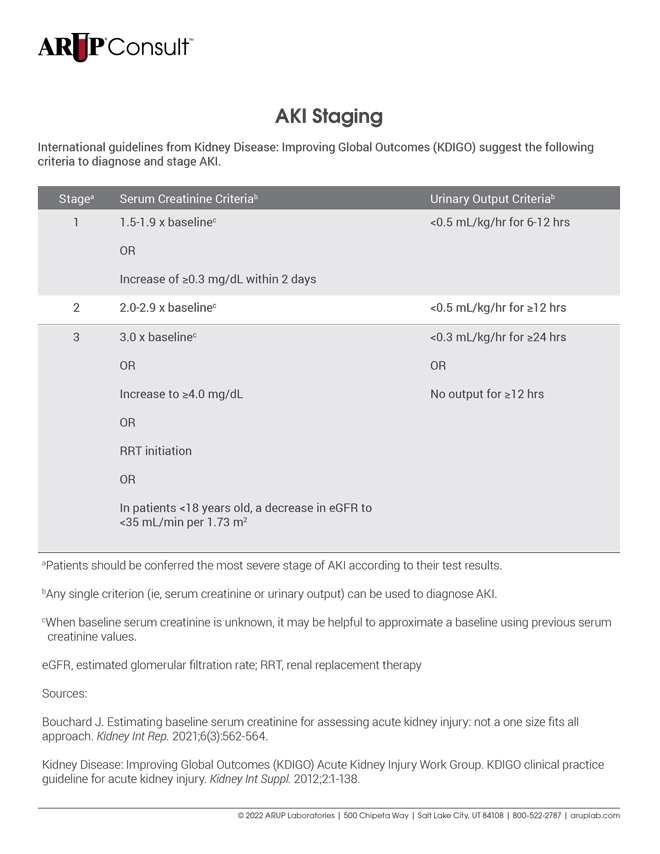
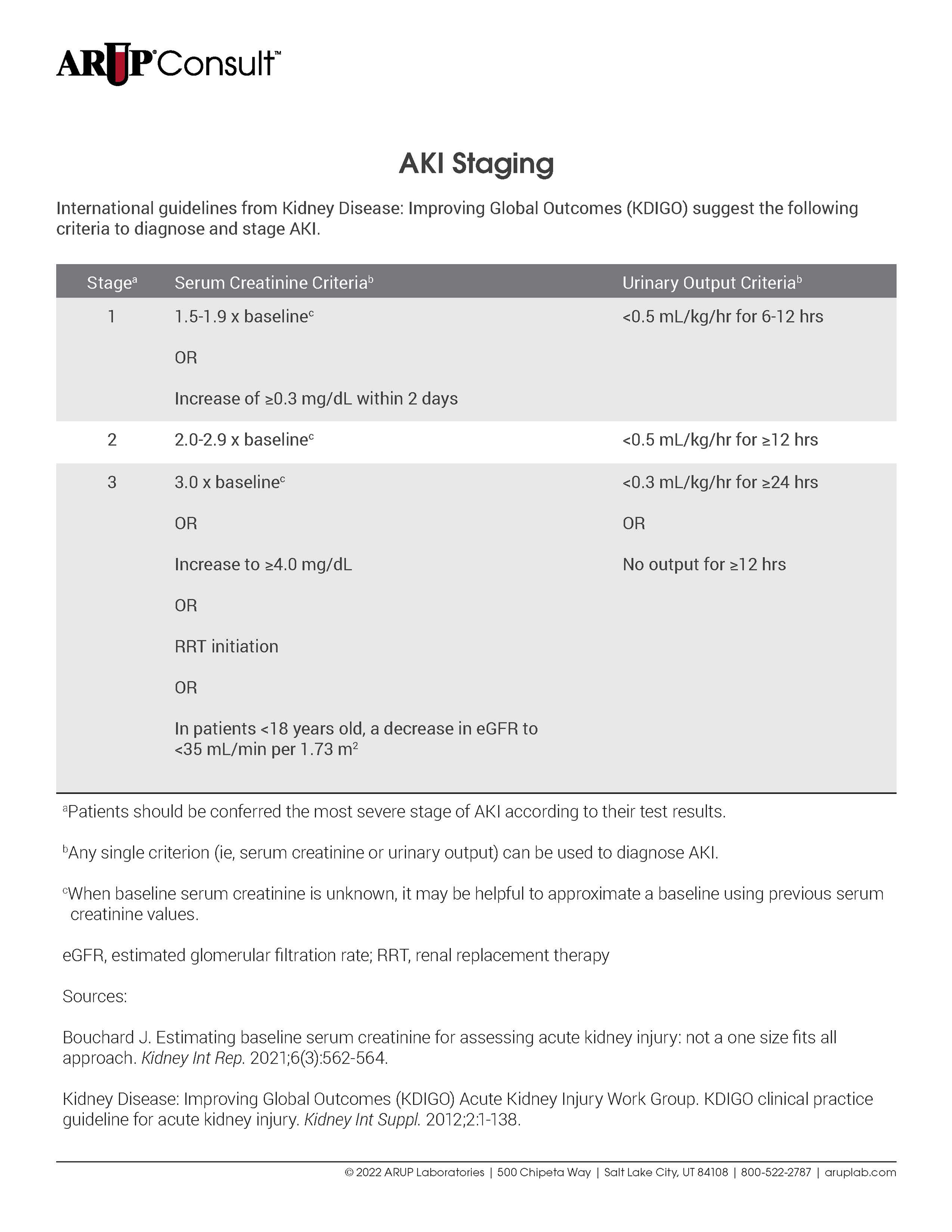
International guidelines from Kidney Disease: Improving Global Outcomes (KDIGO) suggest the following criteria to diagnose and stage AKI.
| Stagea | Serum Creatinine Criteriab | Urinary Output Criteriab |
|---|---|---|
| 1 | 1.5-1.9 x baselinec OR Increase of ≥0.3 mg/dL within 2 days | <0.5 mL/kg/hr for 6-12 hrs |
| 2 | 2.0-2.9 x baselinec | <0.5 mL/kg/hr for ≥12 hrs |
| 3 | 3.0 x baselinec OR Increase to ≥4.0 mg/dL OR RRT initiation OR In patients <18 years old, a decrease in eGFR to <35 mL/min per 1.73 m2 | <0.3 mL/kg/hr for ≥24 hrs OR No output for ≥12 hrs |
aPatients should be conferred the most severe stage of AKI according to their test results. bAny single criterion (ie, serum creatinine or urinary output) can be used to diagnose AKI. cWhen baseline serum creatinine is unknown, it may be helpful to approximate a baseline using previous serum creatinine values. eGFR, estimated glomerular filtration rate; RRT, renal replacement therapy | ||
Some serum creatinine criteria require comparison between test results and a baseline value. However, a baseline value may not be available in cases of acute injury. In such scenarios, it may be helpful to approximate a baseline using previous serum creatinine test results. For additional discussion, refer to Estimating Baseline Serum Creatinine for Assessing Acute Kidney Injury: Not a One Size Fits All Approach.
Follow-Up
Kidney impairment or damage that lasts more than 7 days may denote preexisting or ongoing AKD and should prompt additional consideration. At a minimum, patients with a history of AKI should be reevaluated after 3 months to detect possible CKD. Follow-up testing should include an eGFR and uACR. See the Acute and Chronic Kidney Disease section for specific testing recommendations related to AKD and CKD.
Acute and Chronic Kidney Disease
According to current guidance, AKD can be understood as renal impairment or damage, with or without an occurrence of AKI, that lasts up to 3 months, whereas CKD is renal impairment or damage that persists more than 3 months. AKD or CKD can occur simultaneously with acute injury; when AKI is suspected in the context of existing kidney disease, testing strategies and staging for AKI should be used. ,
Laboratory Testing
When longer-term renal impairment in the absence of AKI is suspected, initial laboratory testing includes serum creatinine, GFR, and uACR (using 24-hour, random, or first-void specimens). Serum cystatin C testing is also recommended during initial assessment so that results are promptly available to confirm GFR.
GFR is often estimated with an equation, such as one of the recommended Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) 2021 equations. Estimated values derived from a serum creatinine measurement (eGFRcr) are recommended for initial evaluation, although direct GFR measurement may be preferred in certain clinical contexts. Direct measurement of GFR is only available through specialized centers.
uACR is the preferred test to detect albuminuria, although the urine protein-to-creatinine ratio (uPCR) may also be used. Reagent strip urinalysis for total protein is less precise than uACR or uPCR and requires laboratory confirmation.
When indicated, confirmatory testing can include eGFR derived from serum cystatin C (eGFRcys) or cystatin C and creatinine (eGFRcr-cys). Clearance measurements of creatinine or exogenous filtration markers can also be used for confirmation. When factors are present that may impact creatinine-based results, cystatin C-based testing should be used.
CKD Diagnosis and Staging
A diagnosis of CKD can be established in patients with a GFR of <60 mL/min/1.73 m2 or at least one marker of structural kidney damage (eg, albuminuria) when impairment lasts for more than 3 months. Additional diagnostic criteria are available for AKD (ie, impairment that lasts up to 3 months); refer directly to KDIGO guidance for more information.
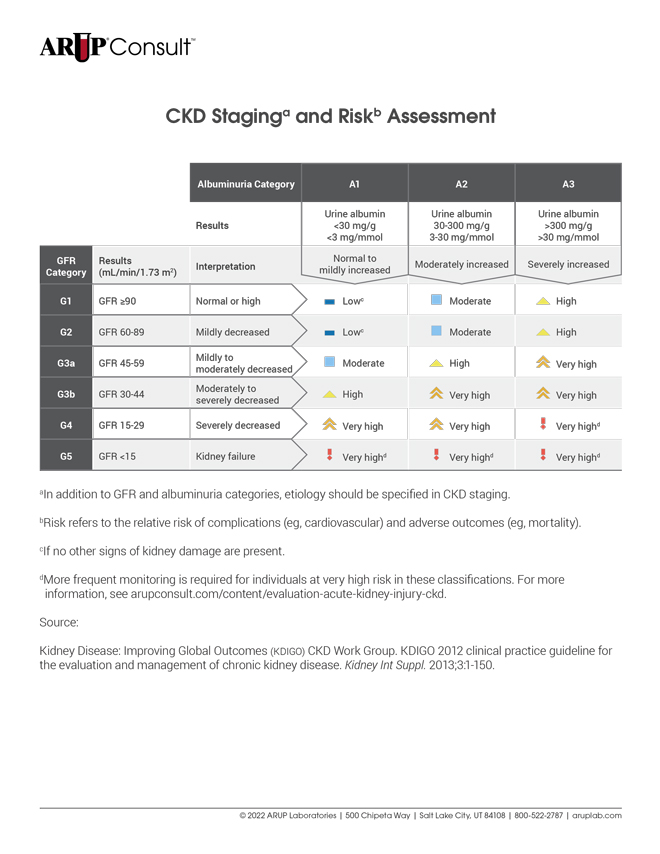
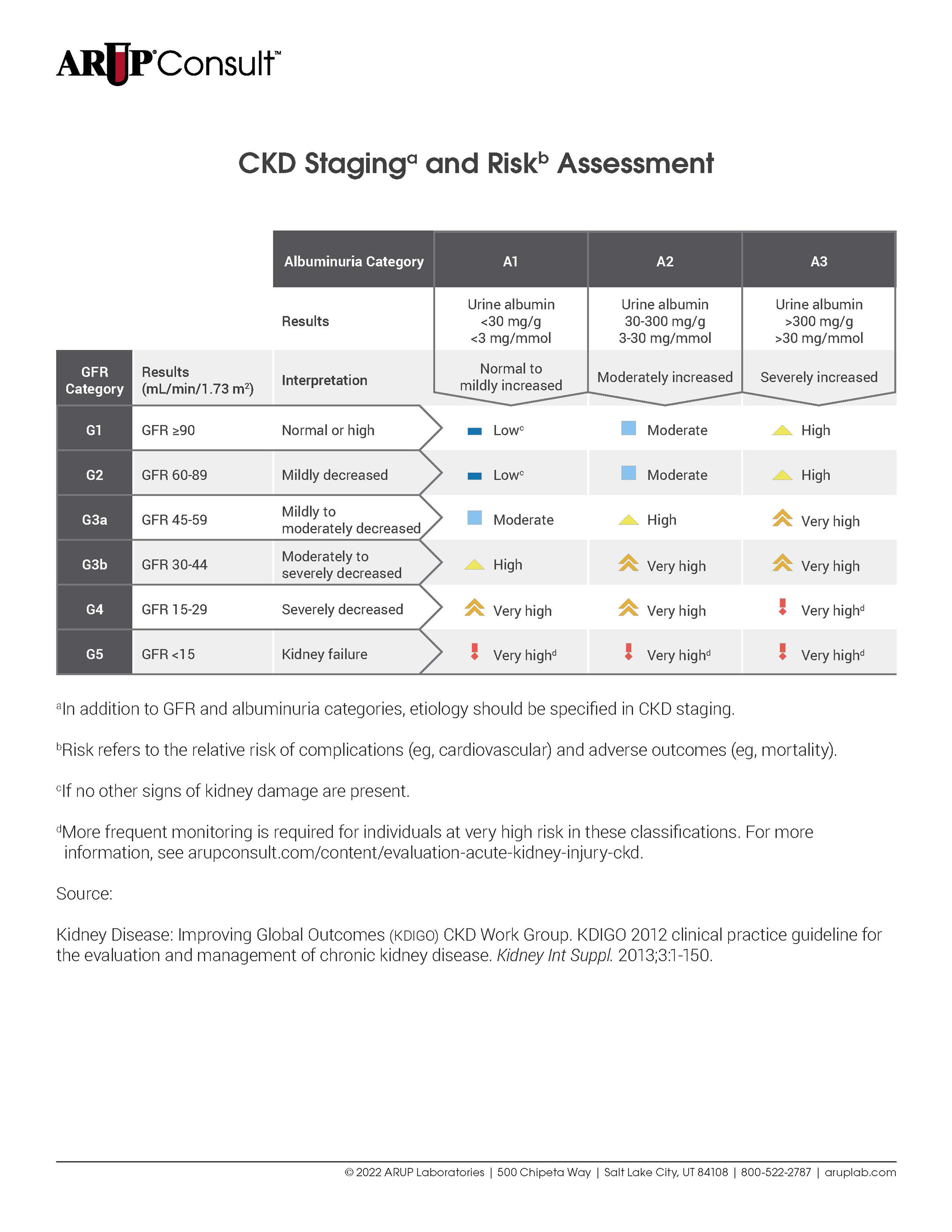
Following diagnosis, staging for chronic disease of the kidneys provides prognostic information, has therapeutic implications, and informs the frequency of monitoring. KDIGO guidelines recommend the following criteria to stage CKD.
| Albuminuria Category | A1 | A2 | A3 | ||
|---|---|---|---|---|---|
| Results | Urine albumin <30 mg/g <3 mg/mmol | Urine albumin 30-300 mg/g 3-30 mg/mmol | Urine albumin >300 mg/g >30 mg/mmol | ||
| GFR Category | Results (mL/min/1.73 m2) | Interpretation | Normal to mildly increased | Moderately increased | Severely increased |
| G1 | GFR ≥90 | Normal or high | Lowc | Moderate | High |
| G2 | GFR 60-89 | Mildly decreased | Lowc | Moderate | High |
| G3a | GFR 45-59 | Mildly to moderately decreased | Moderate | High | Very high |
| G3b | GFR 30-44 | Moderately to severely decreased | High | Very high | Very high |
| G4 | GFR 15-29 | Severely decreased | Very high | Very high | Very highd |
| G5 | GFR <15 | Kidney failure | Very highd | Very highd | Very highd |
aIn addition to GFR and albuminuria categories, etiology should be specified in CKD staging. bRisk refers to the relative risk of complications (eg, cardiovascular) and adverse outcomes (eg, mortality). cIf no other signs of kidney damage are present. dMore frequent monitoring is required for individuals at very high risk in these classifications. See the Follow-Up section for more information. | |||||
Currently, no formal staging criteria exist for AKD. Per expert consensus, CKD staging based on GFR and urine albumin values may be used in AKD without AKI or following AKI; however, data are insufficient to broadly recommend use of CKD criteria in AKD.
Follow-Up
In patients with confirmed CKD, frequency of monitoring using uACR and GFR should be determined based on the risk level (refer to the CKD Staging and Risk Assessment table):
- Low risk (dark blue), test once per year
- Moderate risk (light blue), test once per year
- High risk (yellow), test twice per year
- Very high risk (orange), test three times per year
- Very high risk (red), test four or more times per year
ARUP Laboratory Tests
Quantitative Enzymatic Assay
Quantitative Enzymatic Assay
Quantitative Enzymatic Assay
Quantitative Immunoturbidimetry
Quantitative Enzymatic Assay / Quantitative Immunoturbidimetry
References
-
KDIGO clinical practice guidelines for AKI
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1-138.
-
KDIGO - Clinical practice guideline-chronic kidney disease
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1-150.
-
34252450
Lameire NH, Levin A, Kellum JA, et al. Harmonizing acute and chronic kidney disease definition and classification: report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference. Kidney Int. 2021;100(3):516-526.
-
34918062
Miller WG, Kaufman HW, Levey AS, et al. National Kidney Foundation Laboratory Engagement Working Group recommendations for implementing the CKD-EPI 2021 race-free equations for estimated glomerular filtration rate: practical guidance for clinical laboratories [published correction appears in Clin Chem. 2023;69(4):430]. Clin Chem. 2022;68(4):511-520.
-
34556489
Delgado C, Baweja M, Crews DC, et al. A unifying approach for GFR estimation: recommendations of the NKF-ASN Task Force on reassessing the inclusion of race in diagnosing kidney disease. J Am Soc Nephrol. 2021;32(12):2994-3015.
-
33735329
Bouchard J. Estimating baseline serum creatinine for assessing acute kidney injury: not a one size fits all approach. Kidney Int Rep. 2021;6(3):562-564.


 Cite this page
Cite this page Feedback
Feedback

Estimates are calculated using the 2021 CKD-EPI eGFR creatinine equation